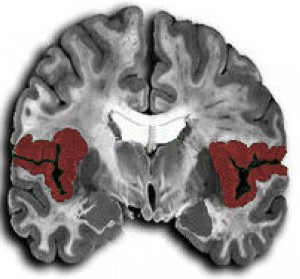
Note the areas shaded in red as they represent the right & left insular cortex.
The insular cortex is thought to be involved in perception, motor control, self-awareness, cognition, and homeostasis by regulating the sympathetic and the parasympathetic nervous systems. It’s also been observed causing ECG abnormalities. (Source literature here, here, here, here,here, and many more)
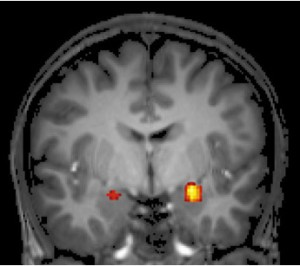
Modern neuroimaging techniques such as functional MRI (fMRI) indicate to us that the insular cortex communicates with the anterior cingulate gyrus and the amygdala to regulate cardiovascular function. The authors of this study propose a neural network (which they call the brain-heart axis) exists.
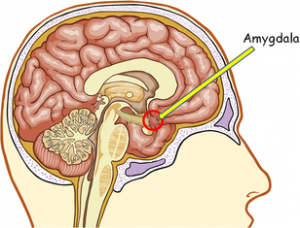
Here’s the amygdala from a side view:
And here’s the right and left amygdala (in each hemisphere) on an fMRI as if you were looking face-to-face with the person being scanned:
The amygdala plays a critical role in emotion which makes it all the more fascinating for it to be implicated in the neural network which helps modulate the heart. It accomplishes this regulation through nerves and neurotransmitters: acetylcholine, norepinephrine, other endogenous catecholamines, & sympathetic/parasympathetic fibers.
So circling back to strokes. If these brain regions affect what goes on in the heart (and what you see on an EKG) then how does a stroke affect them? Enter the middle cerebral arteries (MCA) which supply the vast majority of the blood to the insular cortex regions. Either large MCA strokes, or strokes further down the pipeline into the smaller vessels which supply the insular cortex (and surrounding structures), can cause damage to this network.
Blocked vessels lead to ischemia which leads to circuits failing which leads to dysfunctional regulation which leads to the ECG abnormalities on your cardiac monitor.
Both the Left and the Right insular cortex lesions create problems for the heart however there is greater literature supporting the right insular cortex (supplied by the right MCA and if your patient has a R-MCA blockage affecting the right insular cortex then they would be presenting with symptoms on the left side of the body.) as a far worse culprit.
Abboud, et. al looked at 12 Lead ECG’s from 493 patients which suffered stroke in the right insular cortex as verified by MRI and also 493 control patients then followed both groups for 5 years. Patients with right insular stroke lesions (and in particular those with Long QTc and LBBB on their 12 Lead ECG) showed greater mortality at 2 years. Others have performed similar studies.
It’s important to note, especially in the prehospital setting, that there is presently no consensus on using the ECG to predict lesion location or severity and the utility of even obtaining a prehospital 12 lead during an acute stroke is up for debate. At this point it’s a novelty to help understand the mechanisms of the nervous system but perhaps one day this could materialize into something with serious diagnostic or prognostic value.
Now on to part 3 where we discuss in-depth how the brain can kill (or injure) the heart.









1 Comment
This is interesting information. But so far I haven’t seen a compelling argument for making a 12-lead on a stroke patient a priority. Our treatment does not change knowing where the lesion is. Is does not hasten or delay the patient going to CT once they’re in the ED. What am I missing?
2 Trackbacks